I read this story today and my heart broke a little bit: Couple sues over adopted son’s early sex-assignment surgery.
A South Carolina couple sued doctors and state social workers on Tuesday for subjecting a 16-month-old child born with both male and female genitalia to what they say was medically unnecessary and irreversible sex-assignment surgery while the toddler was in foster care. The state and federal lawsuits — believed by the couple’s lawyers to be the first of their kind in the United States — argue that doctors should not have performed surgery to make the child’s body appear to be female when they knew they could not predict how gender would develop. The child, now 8, has shown strong signs of identifying as male and recently began living as a boy, according to Pam and Mark Crawford, who adopted him after the surgery. Source.
The child in the above story had ambiguous genetalia and was “‘intersex’ / had a ‘disorder of sex development (DSD)’ which is “defined as any congenital condition in which development of chromosomal, gonadal or anatomic sex is atypical” (Source). The child was treated with surgery to make the genitals appear female in February 2005. In August 2006, the American Academy of Pediatrics released a revised Consensus Statement on Management of Intersex Disorders.
While the AAPs recommendations vary based on the exact medical diagnosis, the take-home message is: do what’s best in the long run, not what makes everyone feel most comfortable in the short run, maintain function as much as possible, don’t do anything irreversible that is not required for physical health early on. Some quotes to give you an idea of what they are recommending:
-“Emphasis is on functional outcome rather than a strictly cosmetic appearance. It is generally felt that surgery that is performed for cosmetic reasons in the first year of life relieves parental distress and improves attachment between the child and the parents; the systematic evidence for this belief is lacking.”
-Certain procedures should be delayed until “adolescence when the patient is psychologically motivated and a full partner in the procedure.”
-“Surgical management in DSD should also consider options that will facilitate the chances of fertility.” (Source)
Surgery is a permanent change, is irreversible. What was the young child in that news story robbed of? We cannot tell from the information being released, but at the very least, this child was robbed of a penis.
We may not discuss it much, but these types of conditions are not as rare as you might think. Estimates of the frequency of surgeries to “normalize” genital appearance are as high as 1 in 500 (Source).
The types of conditions are varied and numerous- from chromosomal abnormalities (XXY) to enzyme deficiencies (click here for more info).
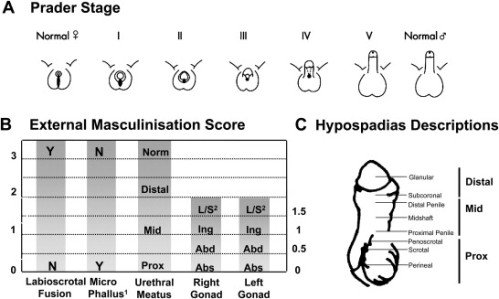
Scoring External Genitalia. A. The external genitalia can be objectively scored using the Prader staging system which provides an overall score for the appearance of the external genitalia. B. Alternatively, each individual feature of the genitalia (phallus size, labioscrotal fusion, site of the gonads and location of urethral meatus) can be individually scored to obtain the External Masculinisation Score (EMS). Adapted from Ahmed et al., BJU Int. 2000;85:120–4. (Source)
The dilemma in how to treat these children is what happens if you choose the wrong gender. What if you get it wrong?
Numerous experts in the field have remarked on the lack of long-term data on how accurate doctors and parents are at choosing the correct gender.
More than 90% of 46XX CAH patients and all 46XY CAIS assigned female in infancy identify as females. … Approximately 60% of 5α-reductase (5αRD2)-deficient patients assigned as female in infancy and virilising at puberty (and all assigned male) live as males… Amongst patients with PAIS, androgen biosynthetic defects, and incomplete gonadal dysgenesis, there is dissatisfaction with the sex of rearing in ∼25% of individuals whether raised as male or female... In the case of mixed gonadal dysgenesis (MGD), factors to consider include prenatal androgen exposure, testicular function at and after puberty, phallic development and gonadal location. Individuals with cloacal exstrophy reared as female show variability in gender-identity outcome, but >65% appear to live as women. Source.
Look at those numbers. In the first case, 10% of patients were assigned the ‘wrong’ gender (i.e. they did not identify themselves as the gender that was chosen for them). In the second, 60% of patients were assigned as female in infancy went on the live as males. The third statistic, 25% of individuals were ‘dissatisfied with the sex of rearing.’ And the last stat, around 35% of individuals reared as females live as males.
If I was a betting individual, I wouldn’t bet on those odds. As a scientist, I see those percentages as indicating that not enough is known about the system to make an accurate prediction of the outcome. As a human being, I mourn for those who lost a part of themselves to surgery that they cannot get back- a part that makes it harder for doctors and surgery to match their outsides with their self-image. As a parent, I imagine how dangerous it would be to make such a decision at the risk of choosing incorrectly.
As I was researching this topic, I came across the following statement that struck me as odd:
Gender reassignment surgery is not carried out prior to adulthood in young gender dysphorics without DSD. There is international clinical consensus that the risks of early surgical intervention far outweigh the potential benefits in virtually all cases. (Source)
Gender dysphoria is when a person feels their biological sex is mismatched relative to the gender they identify as being. The quote above indicates that surgery to bring biological sex in line with gender identity should be delayed until adulthood. Perhaps the same caution should be applied when deciding for infants and young children with disorders of sex determination.
My heart goes out to MC (the child from the story) and his family. May the grownups looking out for him- doctors, parents, lawyers- all do their best, and do what is best for him. May they not fail him twice.


I watched the David Reimer documentary on TLC a long time ago, but I’m still haunted by its conclusion. A voiceover narration reveals that David ultimately committed suicide by shooting himself in the head. The producers followed this segment with David’s final words on camera, “Is it going to take someone to wind up killing themselves — shooting themselves in the head — for people to listen?”
I’m still spooked by it.
I saw the same one. That was kind of what clinched it for me- that if I ever became a parent, I wouldn’t take away any of my child’s options. That poor, poor baby, boy, man.
Great Information about sex assignment surgery in infants young children. Keep posting
We are at Healing Touristry an ISO Certified 9001:2015 Indian healthcare service provider that offers medical treatment to foreign nationals, seeking affordable and safe medical tourism facilities… Click here https://www.healingtouristry.com/